Prevalence of Occupational Skin Diseases and its Predisposing Factors in Leather Tanning Workers of Southern India
Panjakumar Karunamoorthy1
*
 , Rajesh Embiranahalli Mani2
, Beerappa Ravichandran1
, Rajesh Embiranahalli Mani2
, Beerappa Ravichandran1
 , Dhananjayan Venugopal1
, Dhananjayan Venugopal1
 , Mala Ambikapathy1
and Shridhar Jagannath Kondhalkar1
, Mala Ambikapathy1
and Shridhar Jagannath Kondhalkar1
Corresponding author Email: vivepanja@gmail.com
DOI: http://dx.doi.org/10.12944/CWE.15.3.13
Skin diseases are a major occupational health issue in tannery workers because of work related exposure to various toxic chemicals used in tanning process. In the present study, prevalence of various skin diseases and predisposing factors in tannery workers were investigated.A cross sectional study including 114 tannery workers (male-89; female-25) employed at different tanneries of Southern India was carried out. Face to face interview with pre-designed questionnaire and health examination was conducted. Skin samples obtained from the participants were subjected to microscopic examination and microbial culture for diagnosis of skin diseases. The prevalence of occupational skin disorders were 39% among the study participants. Contact dermatitis (16%), skin infections (16%), eczematous lesions (7%) and nail discoloration (1.75%) wereidentified. Skin infections of fungal origin were identified among 11.4% of subjects. The skin infections of fungi; tenia corporis, tenia cruris, tenia unguium, tenia versicolor, tenia pedis and Pityriosis versicolor were identified. Bacterial skin infections identified were associated with contact dermatitis. Lack of PPE usage was reported among 30% of workers. Hazardous working environment, chemical exposure, humidity and lack of PPEusage were significantly associated with increased skin disease incidence(p<0.05), indicating the major predisposing factorsfor Occupation skin diseases.The findings of the study emphasize that,workers in the pre-tanning section and tanning sections are more vulnerable to occupational skin diseases.Compliance to use of PPEs, engineering controls to reduce exposure, education, frequent health surveillance and early identification & treatment could mitigate the occupational skindiseasesamongtannery workers.
Copy the following to cite this article:
Karunamoorthy P, Mani R. E, Ravichandran B, Venugopal D, Ambikapathy M, Kondhalkar S. J. Prevalence of Occupational Skin Diseases and its Predisposing Factors in Leather Tanning Workers of Southern India. Curr World Environ 2020; 15(3). Available from: https://bit.ly/36EvfJl DOI:http://dx.doi.org/10.12944/CWE.15.3.13
Copy the following to cite this URL:
Karunamoorthy P, Mani R. E, Ravichandran B, Venugopal D, Ambikapathy M, Kondhalkar S. J. Prevalence of Occupational Skin Diseases and its Predisposing Factors in Leather Tanning Workers of Southern India. Curr World Environ 2020; 15(3).
Download article (pdf)
Citation Manager
Publish History
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 05-05-2020 |
|---|---|
| Accepted: | 23-10-2020 |
| Reviewed by: | 
 Loai Aljerf
Loai Aljerf
|
| Second Review by: |

 Madhu Gopal
Madhu Gopal
|
| Final Approval by: | Dr Hiren B Soni |
Introduction
The leather tanning industry holds a prominent place in the Indian economy, providing job to 4.42 million people, mostly of lower socio-economic status. Women workers occupy 30% in this sector, among the states Tamil Nadu, the southern part of India holds the major leather production centers. The state of Tamil Nadu is accountable for 60-70% of leather production in India.1Tannery industries are the most toxic in the world owing to intensive chemical usage.The tanning industries involved manual operations, viz; hide handling, soaking, un-hairing, trimming, tanning, dyeing and other finishing process.2 Thus tannery workers exposed to deleterious agents such as acids (Formic acid, sulphuric acid) chromium sulphate, ammonium salts, sodium salts and dyes etc,.3These chemicals are demonstrated as potential irritant and sensitizing agent among worker exposed for long duration.4Chromium salts has potential ability to bind with skin proteins of tannery workers to produce complex antigens which lead to hypersensitivity reactions.5Prevalence of occupational dermatitis has been reported among tannery workers in Asian countries. 6
Occupational skin diseases (OSD) are emerging concern and frequently encounterednotifiable work related health issue. The worsening of pre-existing skin disorders by work related exposures are considered as OSDs which account for 34% of work related diseases.7OSD contributes to the compromised productivity, loss of work days, switch over to other jobs, affects life style, disablement and increased health expenditure among working population.8,9The most important agents responsible for the OSD are chemical, biological, physicaland mechanical factors.10Occupational skin diseases are classified into contact dermatitis, allergic contact dermatitis, contact urticaria, skin cancers, skin infections, skin injuries, pigmentary disorders and miscellaneous types.11Employment in tanneries is probably associated with occupational dermatitis.12
The prevalence of contact dermatitis, urticaria and skin infection, hand eczema, atopic eczema, and bacterial infection were 8%, 7%, 5%, 3%, and 0.5% respectively in the workers of Khartoum tanning industry.13The chemicals used to treat the animal hides have the indistinguishable affect on human skin that disturbs immunological barrier of skin anatomy,14,15consequently it rendered to opportunistic skin infections to the sensitized population. Moist area of the body such as in between the toes, genital area, and underneath the breasts and skin folds are more susceptible to fungal infections.16
Fungal skin infections are usually caused by dermatophytes, non-dermatophytic moulds and commensal yeasts.17Particularly the fungal skin lesions may widespread if left untreated,therefore to treat the fungal skin infections effectively, appropriate laboratory diagnosis is essential for the differentiation of dermatophytosis from other non-mycotic dermatitis.18The inappropriate treatment for tinea infections may progress to chronic, recurrent and multisite infection.9,19. Occupational illness is less likely to be reported in developing countries due to inadequate surveillance programmes.20There are only limited studies on prevalence of infectious skin diseases among the tannery workers, especially of fungal dermatitis. Therefore, the present study designed to investigate the prevalence of occupational dermatitis, associated skin infections and the risk factors responsible for Occupational skin diseases among the tannery workers.
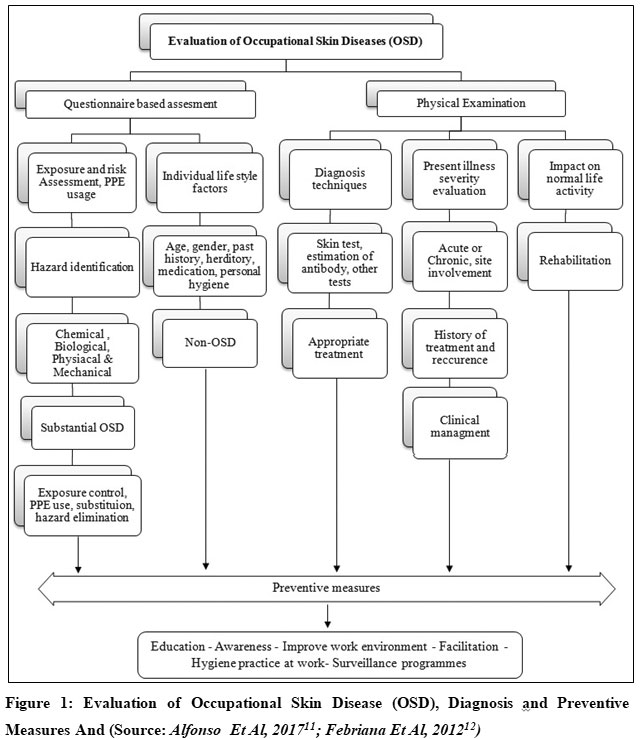 |
Figure 1: Evaluation of Occupational Skin Disease (OSD), Diagnosis and Preventive Measures And (Source: Alfonso Et Al, 201711; Febriana Et Al, 201212) Click here to view figure |
Material and Method
Study Design and Questionnaire
A cross sectional study was conducted to assess the prevalence of occupationalskin diseases among tannery workers. The study was conducted at Southern region of India, included 114 tannery workers (male, n=86; female n=25) with similar socioeconomic strata. Those workers worked in different leather tanning sections, namely pre-tanning section (preparatory), tanning section and post tanning section (finishing) were the study subjects. Institutional ethics committee approval was obtained prior to initiation of the study. A face to face vernacular language (English and Tamil) questionnaire was administered to collect the personal history, personal hygiene practices, socioeconomic status, occupational details, occupational practices specifically related to skin diseases using Nordic Occupational skin disease questionnaire.21
Medical Examination
The clinical examination was conducted to identify the clinical signs and symptoms of contact dermatitis, eczematous lesions, hives, psoriasis, acne, contact allergies, fungal infections (e.g., athlete’s foot, ringworm), bacterial skin infections (with abscesses or exudates), history of atopy or psoriasis, and other skin manifestations . The skin samples were obtained only from the subjectsprovided their consent. Two portions of skin samples were collected from the subjects with skin infection and other skin disorders. From the two portions samples, one portion of sample was examined microscopically with specific staining method and another portion of each sample was cultured onto appropriate medium. The infected skin site was cleaned with 70% alcohol to eliminate the contamination and the skin scales were flaked into sterile petri-plate by using blunt edge sterile surgical blade. Skin scrapings from erythematous lesions and margins of infected skin lesions were aseptically collected. Sterile skin swab moistened with saline was used to collect scanty skin sample and infected lesions.
Sample Collection and Microscopic Observation
A total of 27 skin scrapings and 20 skin swabs were collected from workers. Skin scales collected from workers were subjected to microscopic examination using 10% potassium hydroxide (KOH). Skin scales were taken in a clean and sterile glass slide, and then drop of KOH solution was added onto it. A cover glass placed on the drop and slide was passed three times in a flame to accelerate the dissolving keratin and after a period of 10 minutes, then the cover glass was gently pressed. The presence of fungal elements was examined microscopically under10X (low) and 40X (high) power objectives.
Microbial Culture
Isolation of fungi and bacteria was carried out according to Standard Operating Procedure mentioned inTextbook of Diagnostic Microbiology.22 Samples were cultured by inoculating the scraping pieces over the agar plates. For fungal isolation, the samples were inoculated into Sabouraud’s dextrose agar (SDA) containing cycloheximide and chloramphenicol.23Culture plates were examined for fungal growth.The fungal genus was identified by macroscopic character of culture, microscopic examination of isolates and biochemical characters,22 for macroscopic character colony texture, rate of growth and pigmentation production of the front and the reverse side of the culture plates were observed. Microscopic identification of mould isolates was carried out using lactophenol cotton blue (LPCB). Bacterial culture was performed usingBlood agar (BA) (contained 5% sheep blood) and MacConkey. Smear study, cultural characteristics and biochemical assays were performed to identify the infectious agent from the culture growth.
Statistical Analysis
The resultswere statistically analyzed using SPSS version 26. Descriptive statistics was performed.Chi-square test was used to find the significant association between skin diseases prevalence and other variables. The p-values p< 0.05 was regarded as statistically significant.
Results
Demographic Characteristics and Personal Habits
Demographic characteristics of the workers are presented in Table 1. The mean age of workers was 43.8±10.4 years, ranges from 16 to 68 years. Of the study subjects 26% of them were illiterate, about 45.6% of workers had only primary education, higher secondary education completed by 26.3% workers and only 1.8% of them were graduated. Almost majority of the workers had lowermonthly income varying from Rs.5000 to 8000/- and most of them were temporary employees (95.6%) for several years. Of the study subjects tobacco chewing habits observed among 9.6% subjects, smoking habits reported by 24.6% subjects and alcohol consumption were reported by 36.8% subjects.
Occupational Details
The occupational details of the workers represented in the table 2. According to the working departments of workers, they were proportioned into three groups, about 47.3% of subjects worked in preparatory or pre-tanning process (involved in sorting, curing, storage of hides, soaking, un-hairing, liming, deliming, bating, pickilng and beam house process), 30% of them worked in tanning department (involved in tanning, sammying, and shaving process) and 22% of them involved in post-tanning department (fat liquoring, drying, dyeing and finishing process). The mean work experience of workers was 15.46±10.4 years, ranges from 1 to 36 years. The working hours of the subjects were ranges from 42 to 56 hours/week.
Table 1: Demographic and Occupational Details of Tannery Workers
|
Variables |
Tannery workers (n=114) |
|
|
Age (Years) |
Mean ± SD Range |
43.8±10.4 18-68 |
|
Gender |
Male Female |
89 (78) 25 (21.9) |
|
Marital status |
Married Unmarried |
103 (90.3) 11 (9.6) |
|
Education |
Illiterate Primary Higher Secondary Graduate |
30 (26.3) 52 (45.6) 30 (26.3) 2 (1.8) |
|
Monthly income |
<5000 5000-8000 >8000 |
6 (5.2) 91 (79.8) 17 (14.9) |
|
Job description |
Temporary Permanent |
109 (95.6) 5 (4.3) |
|
Tobacco Chewing |
Chewer Non-chewer |
11 (9.6) 103 (90.3) |
|
Smoking |
Smoker Non-smoker |
28 (24.6) 86 (75.4) |
|
Alcohol consumption |
Alcoholic Non-alcoholic |
42 (36.8) 72 (63.1) |
* Parenthesis indicates percentage (%)
Use of Personal Protective Equipments (PPE’s) were reported among60.5% of subjects and 29.8% of workers did not use any kind of PPE’s, further non-glove users 27.8% and non-apron users 54% were noted. Usage of face mask at work was noted only among 4.3% subjects. The study subjects stated that discomfort while wear, allergic to PPEs, not offeredPPEs by industry, and not able to afford PPEs by self, were the reasons for lackof PPEs use at work. As alternatefor PPEs,workers were reported to be covering the body by self-designed impermeable protectivematerials such as polythene cover and rubber sheets.
Exposure Assessment
Direct handling of chemicals and exposure to chemicals was reported among33% subjects, exposure to dust 36% and experience of high humidity at workplace was reported among 48% (Table 2). The major chemicals reported to be directly handled by the workers were ammonium sulphide, ammonium chloride, sodium chloride, sodium sulphide, sodium metabisulphide, formic acid, sulphuric acid, and chrome sulphatein tanning and in pre-tanning sections (table 5).These chemicals are classified as potential irritant and sensitizing agent to skin and eyes is given in the table 3. These indicate that the workers in pre-tanning and tanning departments are exposed to those chemicals constantly at work.
Table 2: Occupational Details of Study Subjetcs
|
Variables |
Pre tanning (n=54) |
Tanning (n=34) |
Post tanning (n=26) |
Total subjects (n=114) |
|
Worker working section |
54 (47.3) |
34 (29.8) |
26 (22.8) |
114 (100) |
|
Working hours/week
|
16 (29.6) 38 (70.3) |
29 (85.2) 5 (14.7) |
0 26 (100) |
51 (44.7) 63 (55.2) |
|
Work experience
|
32 (59.2) 19 (35.1) 3 (5.5) |
19 (35.1) 12 (22.2) 3 (8.8) |
16 (61.5) 9 (34.6) 1 (3.8) |
67 (58.7) 40 (35) 7 (6.1) |
|
PPE usage
|
43 (83.3) 11 (16.6) 43 (83.3) 38 (70.3) 43 (83.3) 0 2 (3.7) |
25 (73.5) 9 (26.4) 25 (73.5) 25 (73.5) 25 (73.5) 0 3 (8.8) |
21 (80) 15 (57.6) 3 (11.5) 2 (7.6) 1 (3.8) 0 0 |
79 (60.5) 35 (30.7) 71 (62.2) 63 (55.2) 69 (60.5) 0 5 (4.3) |
|
Reason for not wearing PPE
|
5 (9.2) 2 (3.7) 1 (1.8) 3 (5.5) |
3 (8.8) 2 (5.8) 1 (2.9) 3 (8.8) |
7 (26.9) 2 (7.6) 0 6 (23) |
19 (16.6) 11 (9.6) 4 (3.5) 19 (16.6) |
|
Handling of chemicals
|
13 (24) 41(75.9 |
10 (29.4) 24 (70.5) |
3 (11.5) 23 (88.4) |
26 (22.8) 88 (77.1) |
|
Type of exposure
|
19 (35.1) 17 (31.4) 24 (44.4) |
12 (35.2) 3 (8.8) 27 (79.4) |
2 (7.6) 21 (80) 4 (15.3) |
33 (28.9) 38 (33.3) 55 (48.2) |
|
Wearing same clothes repetitively at work |
4 (7.4) |
0 |
4 (15.3) |
8 (7) |
|
*Parenthesis indicates percentage (%) |
||||
|
Dept |
Chemicals used |
Application |
Health effects |
|
Pre-tanning sections
|
Sodium sulphide |
To destroy the hair on hides |
May cause sensitization. Can severely irritate and burn the skin and eyes |
|
Sodium hydrosulphide |
Destroys the hair on hides or skins |
Contact can severely irritate and burn the skin and eyes |
|
|
Sodium hydoxide |
Used in liming process to remove protiens |
Skin irritant: Contact can cause pain, redness, burns, and blistering |
|
|
Ammonium sulphate |
Used to remove alkaline chemicals form skin |
Prolonged skin contact may cause skin irritation and/or dermatitis |
|
|
Ammonium chloride |
Used in deliming process |
Contact can severely irritate the skin and eyes |
|
|
Sodium metabisulphite |
Act as whitening agent in deliming process |
Cause skin and eye irritation |
|
|
Formic acid |
Penetrate into hide and acidify to prepare for tanning process |
Contact can cause pain, burns and ulcers. Eye contact causes pain, watering eyes, and inflammation |
|
|
Sulphuric acid |
To reduce the pH level and acidify the hide |
Contact can cause pain, redness, burns, and blistering. |
|
|
Sodium formate |
Facilitate chromium compound perforation into hide |
Contact can cause skin and eye irritation |
|
|
Tanning section
|
Chromium sulphate |
Penetrates into the collagen matrix during tanning and that stabilize the skin structure |
May cause skin allergy, if allergy develops, can cause itching and skin rash.
|
|
Aldehydes |
Aldehydes are tanning agents used to make wet white |
Irritation of the eyes and skin |
|
|
Post- tanning section |
Dyes |
Dyes are used to give the leather a desired color |
Contact with skin may cause irritation including redness, sores, itching, and burning. |
|
Epoxy resins |
Facilitate high chemical resistance and low water absorption. |
Contact cause skin irritation |
Sources:https://sites.google.com/site/isttschool/useful-information/chemicals-used-in-leather-processing24; http://www.cdc.gov/ niosh/programs.html25
 |
Figure 2: Illustration of Occupational Dermatitis in Tannery Workers (E-F) Click here to view figure |
 |
Figure 3: Illustration of Fungal Dermatitis in Tannery Workers (a-d) Click here to view figure |
Skin Disease Pattern
The medical examination among workers explored about45.6% (n=54) of the study subjects were suffer from skin disorders (Table 4). Skin disorders, viz; Contact dermatitis, allergic dermatitis, seborroheic eczema, seborroheic psoriasis and skin infections were identified among the subjects (Figue 2 &3). The diagnostic pattern to confirm the work related skin diseases (39%; n=44)) among tannery workers is given in figure 4.
Contact dermatitis (15.7%), skin infections (16%), eczematous lesions (6.1%), and nail discoloration (1.7%) were identified as work related skin diseases. The frequency of skin morbidity was found to be high among the workers of pre-tanning and tanning departments. Pickling, liming, and tanning are the major activities that have been reported to be worsen the skin conditions among workers. Sickness absenteeism reported among 32% of workers due to skin disease burden.
Table 4: Skin Disease Profile of the Study Subjects According to their Working Section
|
Variables |
Pre tanning (n=54) |
Tanning (n=34) |
Post tanning (n=26) |
Total subjects (n=114) |
|
Skin diseases prevalence |
34 (62.9) |
14 (41.1) |
4 (15.3) |
52 (45.6) |
|
Types of skin disorders
|
8 (14.8) 3 (5.5) 11 (18.4) 7 (7.4) 5 (1.8) |
4 (11.7) 3 (8.8) 5 (14.7) 1 (5.5) 1 (2.9) |
1 (3.8) 0 2 (7.6) 0 1 (3.8) |
13 (11.4) 6 (5.2) 18 (15.7) 8 (6.1) 7 (3.5) |
|
History of skin disorder |
8 (14.8) 11 (20.3) 6 (11.1) 7 (12.9) 2 (3.7) |
3 (8.8) 4 (11.7) 2 (5.8) 3 (8.8) 2 (2.9) |
2 (7.6) 1 (3.8) 1 (3.8) 0 0 |
13 (11.4) 16 (14.0) 9 (7.8) 10 (8.7) 4 (3.5) |
|
a) Recent skin disease |
||||
|
b) Within the past 3 months |
||||
|
c) Between 3-12 months |
||||
|
d) More than 12 months |
||||
|
e) Only of past history |
||||
|
Seasonal effects in Skin disorder
|
4 (7.4) 28 (51.8) 2 (3.7) - |
4 (11.7) 9 (26.4) 1(2.9) - |
0 4 (15.3) - - |
8 (7.0) 41 (36) 3 (2.6) - |
|
Major activity worsen skin condition a) Liming and pickling b) Tanning c) Dye spray d) Other activities |
19 (35.1) 0 0 15 (27.7) |
0 14 (41.1) 0 0 |
0 0 2 (7.6) 2 (7.6) |
19 (16.6) 14 (12.2) 2 (1.7) 17 (14.9) |
|
Severity of skin disease
|
8 (14.8) 17 (31.4) 9 (16.6) |
2 (5.8) 5 (14.7) 7 (20.5) |
1 (3.8) 2 (7.6) 1 (3.8) |
8 (7) 23 (20.1) 14 (12.2) |
|
Musculoskeletal disorder |
27 (50) |
6 (17.6) |
3 (11.5) |
36 (31.5) |
|
Joint pain |
22 (40.7) |
7 (20.5) |
5 (19.2) |
34 (29.8) |
|
Eye irritation |
5 (9.2) |
3 (5.5) |
1 (3.8) |
9 (7.8) |
|
Sickness absenteeism |
18 (33.3) |
16 (47.0) |
1 (3.8) |
37 (32.4) |
|
*Parenthesis indicates percentage (%) |
||||
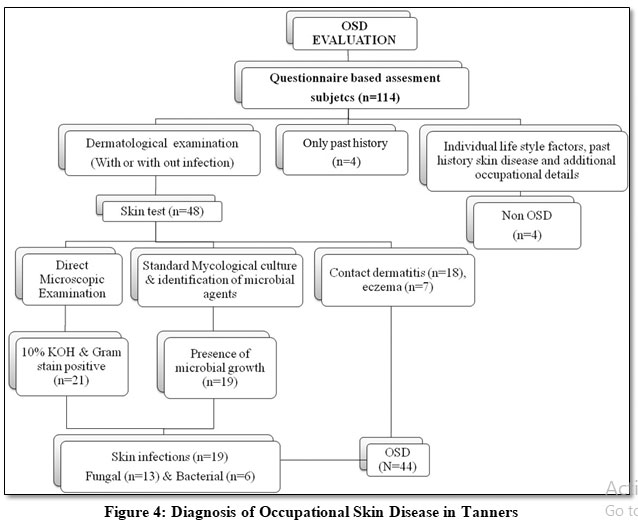 |
Figure 4: Diagnosis of Occupational Skin Disease in Tanners Click here to view figure |
The other health complications of musculoskeletal disorder (32%), joint pain (30%) and eye complaints (8%) were also recorded among workers while performing work.
Skin Infections
Fungal skin infections were identified among 11.4% subjects. The skin infections of; tenia corporis, tenia cruris, tenia unguium, tenia versicolor, tenia pedis and Pityriosis versicolor were identified. The fungal genera of dermatophytes; Trychophyton spp, Microsporum spp, Malassezia spp and non-dermatophtyic fungi; Candida spp,Fusarium spp, Curvularia spp and Aspergillus spp skin infections were identified. Bacterial skin infections were identified among 5.3% of study subjects. Skin infections of Staphylococcus aureus and Klebsiella pneumonia were identified. Bacterial skin infections identified were associated with contact dermatitis.Chronic andrecurrent skin infections were identified among 9.6% (n=11) of study subjects.
The severe skin symptoms of itching, burning sensation, rashes, peeling skin, dry skin, scaling skin and skin lesions were experienced by the subjects. The most affected body sites by the skin disorders are in the order of hand > legs > hip & thigh > groin > foot & toes > face > chest and neck (Figure 5). It was informed by these workers that during summer season the skin infection exacerbate (36%).
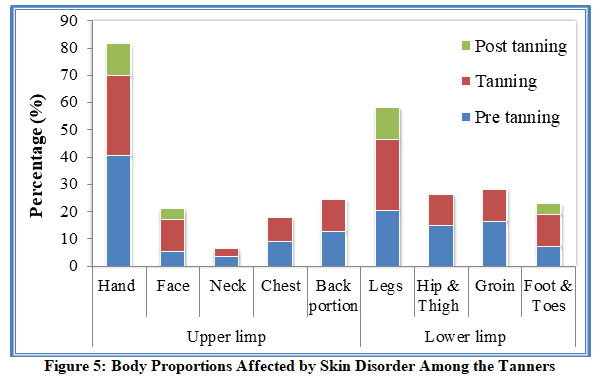 |
Figure 5: Body Proportions Affected by Skin Disorder Among the Tanners Click here to view figure |
Predisposing Factors for Skin Diseases
Chi square test was performed to find the association between skin diseases incidence and the variables of worker’s working section, chemical exposure, dust exposure, humidity, PPE usage, personal habits (tobacco chewing, smoking & alcohol intake), age, monthly income and with work experience (Table 5). The characteristics of working sections, chemical exposure, humidity and lack of PPEs usage were strongly associated with high incident of skin disorders among subjects (p<0.05).
Table5: Predisposing Factors of Skin Disorders Among the Tannery Workers
|
Variables |
Skin disorder n=52 (%) |
p-value |
|
|
Working section |
Pre-Tanning Tanning Post Tanning |
34 (65) 14 (26.9) 4 (7.9) |
0.010* |
|
Age |
≤30 ≤40 >40 |
15 (28.8) 21 (40.3) 18 (34.6) |
0.266 |
|
Gender |
Male Female |
42 (80.7) 10 (19.2) |
0.406 |
|
Monthly income |
<5000 5000-8000 >8000 |
2 (3.8) 39 (75) 8 (15.3) |
0.835 |
|
Tobacco chewing habit |
Yes No |
6(11.5) 46 (88.4) |
0.248 |
|
Smoking habit |
Yes No |
11 (21.1) 41 (78.8) |
0.515 |
|
Alcohol consumption |
Yes No |
18 (34.6) 34 (65.3) |
0.700 |
|
PPE Usage |
Yes No |
47 (90.3) 5 (9.6) |
0.018* |
|
Taking bath after work |
Yes No |
48 (92.3) 4 (7.6) |
0.496 |
|
Hand wash |
Yes No |
50 (96) 2 (4) |
0.871 |
|
Chemical contact |
Yes No |
28 (53.8) 24 (46.1) |
0.001* |
|
Dust exposure |
Yes No |
23 (40.3) 29 (59.6) |
0.143 |
|
Humidity |
Yes No |
39 (75) 13 (25) |
0.001* |
|
Work experience |
1-15 16-30 >30 |
26 (55.4) 18 (34.6) 8 (15.3) |
0.s774 |
|
Sickness absenteeism |
Yes No |
33 (63.4) 19 (36.5) |
0.010* |
|
* p value < 0.05 |
|||
Discussion
Occupational contact dermatitis (OCD) has a significant impact on quality of life, work activity impairment, sickness absenteeism and economic recession.26Present study demonstrated occupational skin diseases prevalence among tannery workers in the study area,which was consistent with the findings of similar studies.13,27-29Likewise, a high prevalence of dermatitis was reported among Kenyan tannery workers.30Dermatophytosis, urticaria, Candidiasis, eczematous lesions and folliculitis were reported among Bangladeshi tannery workers.28A study among tannery workers ofIndonesialeather processing industries showed a prevalence of 7.4% Occupational skin diseases.12Dermatological symptoms of skin rashes, itching and papules were reported among Indian leather tannery workers.27,31Similarly high prevalence of occupational dermatitis was reported among Bangladesh and Sudan tannery workers (67.4%).5,13
The present study reported high prevalence of occupational dermatitis (38%) among tannery workers thanseveralother studies of Indonesia, Kenya, Argentina, Korea and two Indian studies.12,27,31-33. The differences in the workingconditions and the sampling size may also affect the prevalence rate reported among the tanners.12In present study chronic and recurrent skin disorder was found among 10% of workers. Prolonged period of exposure to allergens or irritants associated with recurrent occupational dermatitis.34. This study also found severe skin complications among the workers, which was similarly reported in other studies as occupational aggravate.5,13,35The severity varies on individual physical characteristics including allergen sensitivity, immune capacity and exposure duration to the contaminants.36Occupational factors may play a synergistic role with pre-existing predisposition to allergy.37
In present study the major chemicals reported to be handled by workers in pre-tanning and tanning process aredemonstratedas potential irritant and sensitizer.4 Chromium sulphate, N-diphenylguanidine, benzidine and sodium metabisulfite were demonstrated as sensitizing agent to the exposed workers.12Chromium induced hyper-pigmentation of skin was reported by Al-Hossain et al.38A study found chromate as frequent allergen to tannery workers that increased serum immunoglobulin E (IgE) level.39Workers are exposed to the chemicals while loading, unloading, handling and discarding. The possible exposure routes are inhalation, ingestion and skin absorption. The exposure to chemical agents pose occupational hazard to the workers engaged in these environment, if failed to adopt appropriate personal protective equipments (PPEs).
Present study found 30% of the study subjects did not use any kind of PPE’s atwork, it has been stated that workers who wore gloves were less likely to develop skin diseases compared to those did not wear gloves.40A significant association between lack of PPE use and increased incidents of skindisorder wasdemonstrated in present study (p<0.05). This finding was concordant with the findings of Hasan et al.5In the study area the workers substitutethe unavailability of PPEs with self-designed impermeable protective equipments such as plastic covers and rubber covers. These indicate inappropriate safetypractice at workplace, which increase the chancesofhazard exposure. The rubber gloves used as personal protective equipment can cause leukoderma as reported by Raidas et al.41In developing countries like India the awareness level about health risk and PPE use at workplace are short due to inadequate training.
In the present fungal dermatitis was identified among 11.4% subjects.Few studies reporteddermatophytosis among tannery on dermatological examination.12,28 Present study identified the causative fungal agents in the view of appropriate treatment. The improper treatment for tinea infections may progress to chronic, recurrent, recalcitrant and multisite infection.19The fungal skin lesions may widespread and may impact on social, psychological, and occupational health effects, and the quality of life.42Bacterial skin infections were associated with contact dermatitis in present study. The important predisposing factor for fungal skin infection was wet and humid working conditions. The work environment of pre-tanning and tanning sections were recorded with hot and high humid conditions.12
Present study found that OSD was prevalent amongthe workers involved in pre-tanning and tanning process. These emphasize the workers in pre-tanning sections and tanning sections are prone to health issues due to work place exposure. Occupational skin diseases were high among beam house workers compared with other leather processing departments. During beam house activities the handling of wet hides with bare hand exposed to sulfuric acid, a strongly corrosive agent may cause permanent damage to skin.33Workers with occupational skin diseases (OSD) were significantly correlated with hazardous risk factorsof chemicals contact, inhalation of dust, smoke or vapor, fumes, low and high temperature and humidity.43
Occupational skin diseases among work population are easily treatable and can be preventable, if appropriate preventive measures, workplace improvement and prior training on employment are effectively implemented.
Conclusion
Occupational skin disorders were found to be prevalent among tannery workers. They were followed and treated efficiently. This study also demonstrates the burden of skin disease among tannery workers and its impact on quality of their normal life. Identification of fungal skin infectionsis crucial to prevent chronic and recurrent infections. The study finding emphasizes that pre-tanning section and tanning sections were more susceptible to occupational skin diseases. This working environment serves as a predisposing factor for skin disease morbidity. Obligate use of PPE, workplace improvement, education and frequent surveillance programmes, early identification and treatment could minimize the Occupational skin diseases burden in tannery workers.
Acknowledgements
We are thankful to the Director, ICMR-National Institute of Occupational Health, Ahmedabad for financial support. Authors are also thankful to Dr. Kalaiselvi Kannan, Associate Professor, PSG College of Arts and Science, Coimbatore, Dr. Karthick MD, Christian Medical College, Vellore, Dr. Hariharan MBBS, AFIH, Dr. Subramaniyam, Regenix Superspecialtiy Laboratory, Chennai, Mr. Vijaykumar, Chennai andDr. Jaseer Muhamed, Scientist-B, ROHCS for his comments on manuscript.
Conflict of Interest
The authors declare that they have no competing interests
References
- https://leatherindia.org/indian-leather-industry/
- Aljerf L. High-efficiency extraction of bromocresol purple dye and heavy metals as chromium from industrial effluent by adsorption onto a modified surface of zeolite: Kinetics and equilibrium study. Journal of Environmental Management.2018; 225:120-132.
CrossRef - Hashmi GJ, Dastageer G, Sajid MS, Ali Z, Malik MF, Liaqat I. Leather Industry and Environment: Pakistan Scenario. International Journal of Applied Biology and Forensics. 2017; 1(2):20-25.
- Kolomaznik K, Adamek M, Andel I, Uhlirova M. Leather waste-potential threat to human health, and a new technology of its treatment. Journal of Hazardous Material. 2008; 160(2-3):514-520.
CrossRef - Mahamudul Hasan MD, Hosain S, Asaduzzaman AM, Haque MA and Roy UK. Prevalence of health diseases among Bangladeshi tannery workers and associated risk factors with workplace investigation. Journal of Pollution Effects & Control. 2016, 4:4.
CrossRef - Bhatia R, Sharma VK. Occupational dermatoses: An Asian perspective. Indian Journal of Dermatology, Venereology and Leprology. 2017; 83: 525-35.
CrossRef - Diepgen TL Kanerva L. Skin diseases in Europe. Eur I Dermatol 2006; 16:324- 330.
- Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: a comprehensive review. Indian Dermatology Online Journal. 2016; 7(2); 77-86.
CrossRef - Rajagopalan M, Inamadar A, Mittal A, Miskeen AK, Srinivas CR, Sardana K, Godse K, Patel K, Rengasamy M, Rudramurthy S, Dogra S. Expert Consensus on the Management of Dermatophytosis in India (ECTODERM India). BMC Dermatology. 2018; 24; 18(1):6.
CrossRef - National Institute for Occupational Safety and Health (NIOSH). Online pocket guide to chemical hazards. Appendix C, Centers for Disease Control and Prevention, USA; 2015. Available from: http://www.cdc.gov/ niosh/programs.html.
- Alfonso JH, Bauer A, Bensefa-Colas L, Boman A, Bubas M, Constandt L, Crepy MN, Goncalo M, Macan J, Mahler V, et al. Minimum standards on prevention, diagnosis and treatment of occupational and work-related skin diseases in Europe - position paper of the COST Action StanDerm (TD 1206). Journal of the European Academy Dermatology Venereology. 2017; 31(4):31-43. doi: 10.1111/jdv.14319.
CrossRef - Febriana SA, Jungbauer F, Soebono H, Coenraads PJ. Inventory of the chemicals and the exposure of the workers’ skin to these at two leather factories in Indonesia. International Archivesof Occupational Environmental Health. 2012; 85: 517-526.
CrossRef - El-Hassan KE, El-Kordofani YM., Mithani A, Tayseer E. E D, Zuhair A A B, Ali Thoulifkar A I, Gamal O, et al. The Prevalence of Occupational Dermatosis among Workers in Khartoum State’s Tanneries. American Journal of Dermatology and Venereology. 2014, 3(5): 81-83.
- Klimová Z, Hojerová J, Lucová M and Silvia Pažoureková S. Dermal exposure to chemicals - evaluation of skin barrier damage. Acta Chimica Slovaca, 2012; 5(1): 70-74.
CrossRef - Febriana SA, Soebono H, Coenraads PJ. Occupational skin hazards and prevalence of occupational skin diseases in shoe manufacturing workers in Indonesia. International Archives of Occupational Environmental Health. 2014; 87:185-94.
CrossRef - Aaron DM. Overview of fungal skin infections. Merck Manual Consumer Version website. www.merckmanuals.com/home/skin-disorders/fungal-skin-infections/ overview-of-fungal-skin-infections. 2017. 15.
- Gupta CM, Tripathi K, Tiwari S, Rathore Y, Nema S, Dhanvijay AG. Current trends of Clinico mycological profile of Dermatophytosis in Central India. IOSR-Journal of Dental and Medical Sciences. 2014; 13(10):23-6.
CrossRef - Pihet M, Le Govic Y. Reappraisal of conventional diagnosis for dermatophytes. Mycopathologia. 2017; 182(1-2):169-80.
CrossRef - Dogra S, Uprety S. The menace of chronic and recurrent dermatophytosis in India: is the problem deeper than we perceive? Indian Dermatology Online Journal. 2016; 7(2):73-76.
CrossRef - London L, Kisting S (2002) Ethical concerns in international occupational health and safety. Occup Med 17(4):587-600.
- Shamout Y and Adisesh A. The Nordic Occupational Skin Questionnaire. Occupational Medicine. 2016; 66(1): 82. https://doi.org/10.1093/occmed/kqv059.
CrossRef - Mahon CR and Donald C Lehman DC. Textbook of Diagnostic Microbiology 6th edition. 2018. ISBN: 9780323613170. Pages?
- Scognamiglio T, Zinchuk R, Gumpeni P, and Larone DH. Comparison of inhibitory mold agar to Sabouraud Dextrose Agar as a primary medium for isolation of fungi. Journal of Clinical Microbiology. 2010; 48(5): 1924-1925.
CrossRef - https://sites.google.com/site/isttschool/useful-information/chemicals-used-in-leather-processing
- http://www.cdc.gov/ niosh/programs.html
- Kalboussi H, Kacem I, Aroui H, ElMaalel O, Maoua M, Brahem A, El Guedri S, Chatti S, Ghariani N, and Mrizak N. Impact of Allergic Contact Dermatitis on the Quality of Life and Work Productivity. Dermatology Research and Practice. 2019, 3797536, 8. doi.org/10.1155/2019/3797536.
CrossRef - Rastogi SK, Pandey A and Tripathi S. Occupational health risks among the workers employed in leather tanneries at Kanpur. Indian J Occup Environ Med. 2008; 12(3): 132-135.
CrossRef - Rahman M, Akhtar N, Ahmed BN, Hassan KM, Nahar K, Paul HK, Islam MT, Shahidulla AZM, Islam S. Skin diseases in tannery workers of Hazaribagh, Dhaka, Bangladesh: A cross sectional study. Bangladesh J. Dermatol. Venerol. Leprol. 2007; 24(1): 15-20.
- Islam R, Hossain S and Siddique AB. Occupational health hazards and safety practices among the workers of tannery industry in Bangladesh. Jahangirnagar UniversityJournal of. Biological. Sciences. 2017, 6 (1): 13-22.
CrossRef - Were F, Moturi M, Wafula G. Chromium exposure and related health effects among tannery workers in Kenya. Journalof Health and Pollution. 2014; 4:25-35.
CrossRef - Shukla A, Kumar S, Ory FG. Occupational health and the environment in an urban slum in India. Social Scienceand Medicine. 1991; 33(5):597-603.
CrossRef - Kvitko E. Occupational contact dermatitis in the tanning industry. Contact Dermatitis. 2001; 45(4):256.
CrossRef - Ory FG, Rahman FU, Katagade V, Shukla A, Burdorf A. Respiratory disorders, skin complaints, and low-back trouble among tannery workers in Kanpur, India. American Industrial Hygiene Association Journal. 1997; 58(10):740-746.
CrossRef - Schwensen JF1, Menné T, Veien NK, Funding AT, Avnstorp C, Østerballe M, Andersen KE, et al. Occupational contact dermatitis in blue-collar workers: results from a multicentre study from the Danish Contact Dermatitis Group (2003-2012). Contact Dermatitis. 2014; 71:348-55.
CrossRef - Mohanta MK, Saha AK and Hasan MA. Rajshahi: Prevalence and determination of occupational diseases of leather tannery workers. University Journal of Zoology. 2012; 31: 79-82.
CrossRef - Castellanos-Arévalo DC, Castellanos-Arévalo AP, Camarena-Pozos DA, Colli-Mull JG, Maldonado-Vega M. Evaluation of Microbial Load in Oropharyngeal Mucosa from Tannery Workers. Safety and Health at Work. 2015; 6(1): 6.
CrossRef - Shahzad K, Akhtar S and Mahmud S. Prevalence and determinants of asthma in adult male leather tannery workers in Karachi, Pakistan: A cross sectional study. BMC Public Health. 2006, 6:292.
CrossRef - Al-Hossain MM, Ichiro Y, Huadong Xu, Saheduzzaman, Nobutaka OG, Nazmul A, AZim AA, Masashi K. Chromium-mediated hyperpigmentation of skin in male tannery workers in Bangladesh. Chemosphere. 2019; 229. 611-617.
CrossRef - Zareen S, Rehman HU, Zaman H, Ali T, Rashid L, Jamal B, Saeed FK. Occupational allergic contact dermatitis in tannery workers of Peshawar KP Pakistan: an under estimate health issue. Journal of Entomology and Zoology Studies. 2016; 4(5): 310-312.
- Schmidt K, Kersten N and Pohrt U. The use of protective gloves in occupational skin disease prevention: feasibility and customer ascceptance in physiotherapy. Int J Physiother. 2016; 3(4), 401-408.
CrossRef - Raidas RB. Occupational health hazards in tanneries. Directorate general factory advice service & labour institutes, Mumbai, India. Indoshnews. 2007; 2: 4-7.
- Jerajani H, Janaki C, Kumar S, Phiske M. Comparative assessment of the efficacy and safety of Sertaconazole (2%) cream versus terbinafine cream (1%) versus Luliconazole (1%) cream in patients with Dermatophytoses: a pilot study. Indian J Dermatol. 2013; 58(1):34-8.
CrossRef - Park JS, Park EK, Kim HK, Choi GS. Prevalence and Risk Factors of Occupational Skin Disease in Korean Workers from the 2014 Korean Working Conditions Survey. Yonsei Med J. 2020; 61(1):64-72. doi: 10.3349/ymj.2020.61.1.64.
CrossRef






